In line with the ADA’s Well being Coverage Institute File, 65% of American citizens have dental insurance coverage or dental advantages. That suggests maximizing well timed compensation from insurance coverage carriers is very important to wholesome earnings cycle control, money go with the flow, and apply profitability. The caliber of your dental billing processes, the cleanliness of your declare submissions, and your diligence with appeals will decide how effectively you achieve this objective.
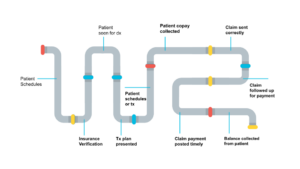
The earnings cycle pipeline begins the instant a affected person schedules an appointment and ends when the affected person steadiness is accumulated. All the pipeline contains each step in-between the beginning and end. Throughout the pipeline, alternatives exist for cracks, leaks, and stoppages to happen. You’ll save you those from going down by means of following those 5 confirmed methods that lend a hand streamline an place of job’s dental billing processes. By way of doing so, you’re going to be nicely in your strategy to gathering all this is rightfully owed on your apply within the shortest time imaginable.
-
Expand a Pre-appointment Readiness Plan
It’s possible you’ll suppose the preparation and submission of claims is all performed on the again finish. However claims can’t be blank except thorough and whole data is collected at the entrance finish – even sooner than you spot the affected person.
Put a pre-appointment readiness plan in position. This is helping make certain that correct affected person and subscriber data is accumulated, insurance policy is verified, and the whole thing is entered into the PMS sooner than the affected person arrives for his or her appointment. With out this procedure in position, time and assets are wasted chasing down, verifying, and correcting data in a while. Those distractions lengthen declare submissions.
By way of imposing a pre-appointment readiness plan, you’ll save you the next commonplace errors that regularly lead to delays and denials:
- Record the affected person’s recurrently used title as a substitute of prison title (e.g., Invoice as a substitute of William, or center title if usually used)
- Record the flawed location if the insurer has more than one places
- Learning after the reality the affected person has clinical however no longer dental protection
Analyze the most typical reasons of denials happening at your apply. Then, incessantly enhance your readiness plan so that you can cope with as many as imaginable at the entrance finish. This may occasionally enhance your declare compensation good fortune fee.
Pre-appointment Readiness Plan Tick list
- Agenda affected person with the proper supplier
- Download affected person insurance coverage data previous to appointment
- Check insurance policy 2-3 days sooner than appointment (or let eAssist’s Insurance coverage Verification products and services maintain that!)
- Insurance coverage verification breakdown finished & entered into PMS
-
Connect the proper CDT code to the provider equipped
Having accumulated whole and correct affected person and insurance coverage data previously, now it’s time to serve your affected person. As soon as once more, correct data is the most important to fighting leaks and stoppages to your earnings cycle pipeline.
The golden rule of dentistry is to all the time code for what you do. However that may be more straightforward stated than performed. As lined within the prior phase, code adjustments, additions, and deletions are made annually (and every now and then mid-year) – and feature totaled 160 prior to now 3 years!
With out essentially the most up-to-date coding assets, you can’t know in case your submissions are correct, which ends up in delays, denials, and misplaced earnings from lowered or flawed compensation. This additionally places the apply in danger for insurance coverage audits.
“Proper coding regularly leads to upper earnings, as practices download reimbursements that have been as soon as unpaid as a result of false impression or misreported codes.” — Dr. Charles Blair
PRO TIP: Making an investment in present, whole, and correct coding reference fabrics each and every 12 months will enhance declare compensation, remedy making plans, and extra. Teach the entire staff and be up-to-the-minute.
-
Download all essential scientific documentation
Correct CDT codes, the precise suppliers, and correct affected person and insurance coverage data aren’t all which are required for blank claims. For a declare to be blank, it should have thorough and whole scientific notes and documentation captured at time of provider.
Medical notice templates lend a hand stay claims squeaky blank. The ADA recommends the usage of the SOAP structure to lend a hand be sure that scientific notes comprise whole main points in regards to the affected person’s dental wishes, diagnoses, and remedy.
Sidebar:
| S | SUBJECTIVE – What the affected person introduced with
In keeping with or influenced by means of private emotions, tastes, or critiques |
| O | OBJECTIVE – What the physician noticed
One thing this is with out bias; factual observations |
| A | ASSESSMENT – What the physician identified
The analysis or estimation of the character, high quality or skill of anyone or one thing |
| P | PLAN – Remedy plan and subsequent appointment
An in depth proposal for doing or reaching one thing |
A blank declare has the entire essential documentation hooked up to entirely improve the remedy equipped. Merely put, the remedy is much more likely to be deemed essential within the eyes of the insurance coverage provider when each the what and the why in the back of it are obviously outlined.
That stated, submissions should be concise and well-organized. Your function is to supply the whole thing the insurance coverage corporate want and desires, however with out going overboard. Offering long explanations that get complicated, placing too many characters into the “narrative” field (which simply get truncated), or attaching an excessive amount of data can paintings in opposition to you. Your staff will spend additional time getting ready over the top submissions, best to have them kicked again as a result of they have been unclear and complicated. They’ll then wish to spend much more time condensing and resubmitting a clearer declare, the entire whilst negatively impacting your collections.
| Examples of essential supportive scientific documentation that successfully hits the mark: | |
|
|
On the other hand, even the most productive scientific notes received’t lead to a briefly paid declare compensation if the notes aren’t signed by means of each the rendering supplier AND the hygienist or dental assistant. A easiest apply is to digitally chart the whole thing, and maximum Follow Control Methods permit for virtual signatures.
-
Ship blank number one and secondary claims
At the back of faulty codes, the second one maximum commonplace reason for declare rejections and denials is flawed data – which is fully avoidable. As soon as glad that each element has been reviewed for accuracy, and the declare package deal is blank and whole, you’re in a position to put up to the insurance coverage provider.
Claims is also despatched by means of mail or fax, however a easiest apply is to put up electronically when to be had. Amongst different advantages, this permits you to invoice the affected person for balances due in a extra well timed way, so you might be additionally optimizing affected person earnings.
Any other easiest apply is to ship claims day by day. On the other hand, don’t suppose the tip of the day is the most productive time. Many practices to find that filing claims the following industry morning lets in for higher center of attention and focus to get the entire main points excellent. Decide what works easiest in your place of job and your staff.
PRO TIP: Sending blank claims day by day guarantees well timed declare compensation. This is helping stay sufferers feeling safe to your apply’s talents – and boosts retention.
Relating to a secondary declare, connect a duplicate of the main EOB that presentations the quantity paid by means of the main payer. Use the “remarks” field to checklist number one provider and paid quantity so advantages can also be correctly coordinated. As a part of your pre-appointment readiness plan, remember to are gathering date of delivery for each affected person and subscriber. As an example, you’re going to want this knowledge when a kid affected person is underneath the father or mother’s coverage, or when coping with twin insurances. Maximum carriers apply the DOB rule when figuring out which coverage is number one and which is secondary, so gathering that data we could YOU know which is the main declare.
-
Toughen the attraction procedure (when appropriate)
In line with business chief and dental coding professional, Dr. Charles Blair, best about one-third of denied claims are appealed. Workforce capability is also the barrier, and/or staff participants lack the data about why, when, and the best way to record an attraction.
Does YOUR dental biller know when to attraction or no longer attraction?
- Rejected claims should be reviewed for accuracy, corrected, and resubmitted. Rejected claims are essentially the most irritating – and maximum avoidable – roadblock to well timed compensation. All the time attraction!
- Disallowed claims for disallowed procedures (according to the EOB) aren’t billable to the affected person and must be written off. As disappointing as those are for the suppliers and the apply, they’re particularly irritating for the affected person when the result’s an sudden steadiness due. On the other hand, relying at the explanation why given, some must be appealed.
- Denied claims are kicked again for a explanation why, which shall be said at the EOB. If because of lacking information or submitting mistakes, no doubt attraction. In the end, relying at the explanation why given, many must be appealed.
Analyze all of your claims which are being kicked again and determine patterns within the causes given at the EOBs. E.g., persistently lacking the similar data, sure CDT codes incessantly misused, loss of enough documentation, or lacking signatures. Proper your processes to mend those leaks to your earnings cycle pipeline.
In conclusion, you’ll building up declare reimbursements – and in the long run earnings – via the next steps. 1) broaden a pre-appointment readiness plan, 2) connect the proper CDT code to the provider equipped, 3) download all essential scientific documentation, 4) ship blank number one and secondary claims, and 5) improve the attraction machine.
Dental insurance coverage billing is a time-consuming procedure that calls for revel in to get proper. When you’re suffering with getting claims paid, imagine outsourcing via a relied on dental billing platform. Click on right here to time table a complimentary session.